Learning Objectives
- Identify the locations and functions of the chambers and valves of the mammalian heart
- Trace the complete path of blood flow through the mammalian heart
- List the steps of the mammalian cardiac cycle, identify when each chamber is in diastole or systole at each point of the cycle, and identify when valves are open or closed at each point in the cycle
- Describe the process of electrical activation of the cardiac cycle, and identify the roles of the nodes essential for electrical conduction pathways
- Identify the physical and electrical activities of the cardiac cycle along each point on an ECG
- Identify and describe processes that affect heart rate, blood pressure, and cardiac output
Structures and Functions of the Mammalian Heart
The information below was adapted from OpenStax Biology 40.3
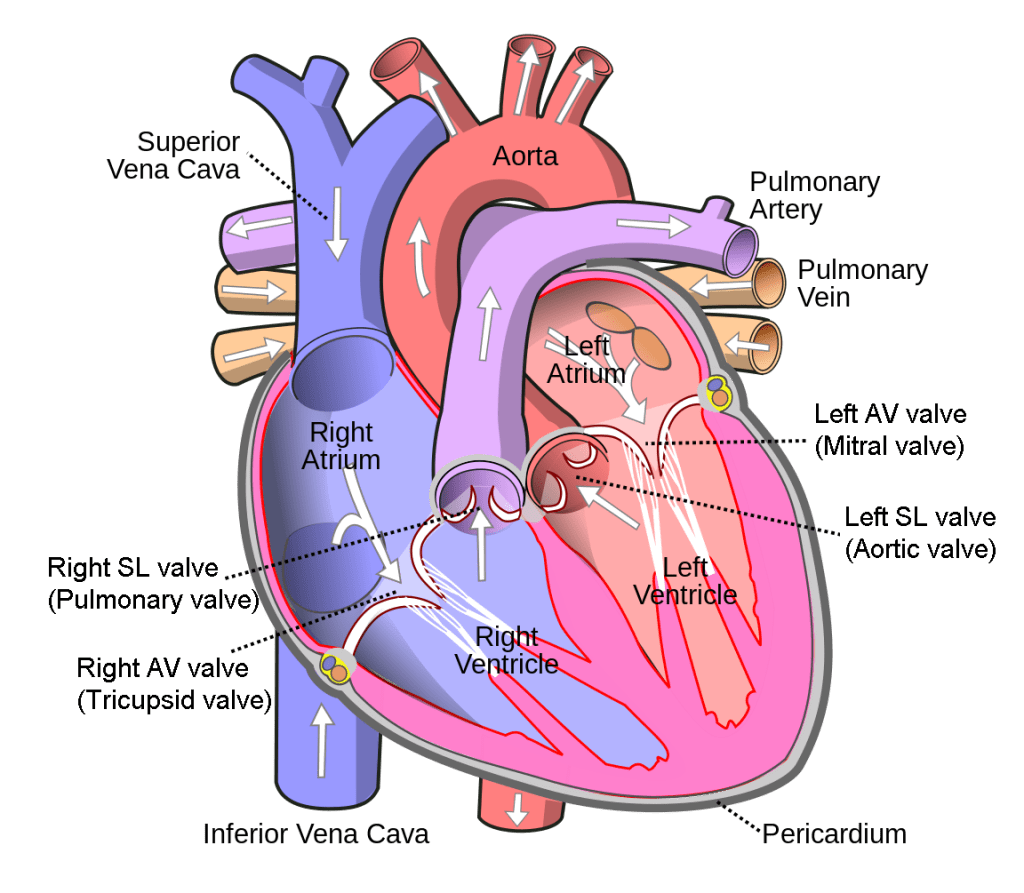
The mammalian heart is a four-chambered muscle that pumps blood through the lungs to acquire oxygen and expel carbon dioxide, and to the body to deliver oxygen and collect carbon dioxide waste. Each side of the heart has one atrium at the top (where blood enters the heart), and one ventricle at the bottom (where blood is pumped out of the heart). A set of one-way valves, called atrioventricular (AV) valves, separate each atrium and ventricle to prevent backflow of blood; another set of valves, called semilunar (SL) valves, separate each ventricle from its associated artery.
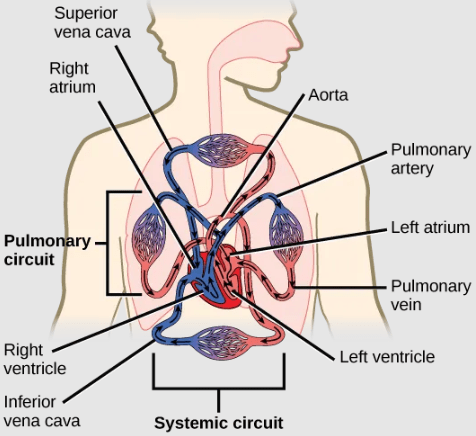
The heart muscle is asymmetrical as a result of the distance blood must travel in the pulmonary and systemic circuits. Since the right side of the heart sends blood to the pulmonary (lung) circuit, it is smaller than the left side which must send blood out to the whole body in the systemic (body) circuit.
Path of Blood Through the Mammalian Heart
The information below was adapted from OpenStax Biology 40.3
As noted above, the mammalian heart has one atrium and one ventricle on the right side, and one atrium and one ventricle on the left side. The atria are the chambers that receive blood, and the ventricles are the chambers that pump blood. Blood follows a complete double circuit through the heart as described below:
- The right atrium receives deoxygenated blood from the systemic (body) circuit from two large veins, the superior vena cava and the inferior vena cava.
- This deoxygenated blood then passes to the right ventricle through the right atrioventricular valve (tricuspid valve), a flap of connective tissue that opens in only one direction to prevent the backflow of blood.
- After it is filled, the right ventricle pumps the blood through the pulmonary arteries, passing through the right semilunar valve (pulmonic valve) to the lungs for re-oxygenation.
- After blood passes through the pulmonary arteries, the right semilunar valves close preventing the blood from flowing backwards into the right ventricle.
- The left atrium then receives the oxygen-rich blood from the lungs via the pulmonary veins.
- The oxygenated blood passes through the left atrioventricular valve (bicuspid valve or mitral valve) to the left ventricle.
- After it is filled, the left ventricle pumps blood out through aorta, the major artery of the body, taking oxygenated blood to the organs and muscles of the body, passing through the left semilunar valve (aortic valve) to the body.
- Once blood is pumped out of the left ventricle and into the aorta, the left semilunar valve closes to prevent blood from flowing backward into the left ventricle.
This video describes the structure and function of the human heart:
The Mammalian Cardiac Cycle
The information below was adapted from OpenStax Biology 40.3
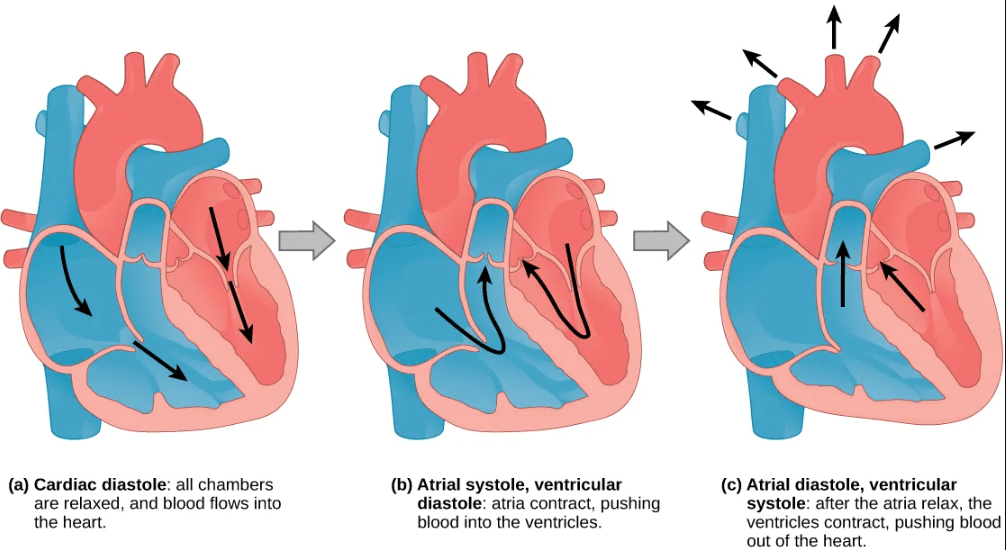
The main purpose of the heart is to pump blood through the body; it does so in a repeating sequence called the cardiac cycle. The cardiac cycle is the coordination of the filling and emptying of the heart of blood by electrical signals that cause the heart muscles to contract (systole) and relax (diastole):
- Before the start of the cardiac cycle, the heart is in a stage called cardiac diastole, when all four chambers of the heart are relaxed. Cardiac diastole allows blood to flow into the heart unimpeded; the AV valves are open, and the SL valves are closed during this stage.
- The first step of the cardiac cycle is atrial systole, the atria contract and push blood into the ventricles. The ventricles are still experiencing diastole (relaxation) during atrial systole. The AV valves are open to allow blood to pass from the atria to the ventricles, and the SL valves remain closed to prevent backflow of blood into the ventricles from the arteries.
- The next step of the cardiac cycle is ventricular systole, when the atria relax (atrial diastole), and the ventricles contract to push blood out of the heart. The AV valves close to prevent backflow from ventricles to atria, while the SL valves open to allow blood to exit the ventricles into the arteries; closing of the atrioventricular valves produces a monosyllabic ‘lub’ sound (first heart sound).
- In the final stage of the cardiac cycle, the heart the enters cardiac diastole, when both atria and ventricles are relaxed. The SL valves close and complete the cardiac cycle; closing of the SL valves produces a monosyllabic ‘dub’ sound (second heart sound).
This video describes the cardiac cycle in the human heart:
Electrical Activity Regulates the Cardiac Cycle
The information below was adapted from OpenStax Biology 40.3
The heart is composed of specialized muscle cells called cardiomyocytes, and the cardiac cycle is caused by the coordinated contraction of cardiomyocytes throughout the heart at the appropriate time. Cardiomyocytes have properties in between skeletal and smooth muscle: cardiomyocytes are striated like skeletal muscle, but they pump rhythmically and involuntarily (without nervous system stimulation) like smooth muscle. The involuntary contraction of cardiomyocytes is mediated by special structures called intercalated discs, which spread membrane depolarization (and thus contraction) from one cardiomyocyte to the next. Isolated cardiomyocytes will even contract autonomously in a petri dish, if given the correct balance of nutrients and electrolytes.
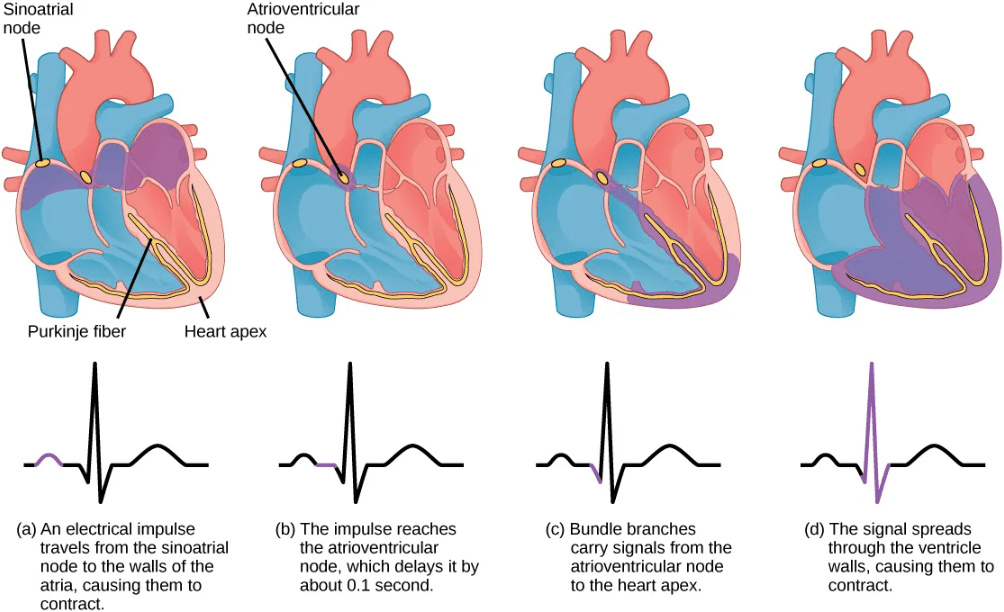
The coordinated contraction of cardiomyocytes is regulated by a series of specialized cells and structures at various locations in the heart:
- A group of cells called pacemaker cells are responsible for initiating the cardiac cycle. The pacemaker cells are located at a site called the sinoatrial (SA) node, at the upper back wall of the right atrium just below the location where the superior vena cava joins the right atrium.
- The pacemaker cells depolarize autonomously, creating a specialized action potential or electrical pulse called a cardiac action potential.
- The cardiac action potential spreads through the two atria via the intercalated discs that link the cardiomyocytes, causing the two atria to contract in unison.
- As the atria contract, the cardiac action potential reaches a second node called the atrioventricular (AV) node, located between the right atrium and right ventricle. The atrioventricular node “pauses” the cardiac action potential for approximately 0.1 second before it then spreads to the walls of the ventricles. This pause allows the atria to empty completely into the ventricles before the ventricles contract to pump out the blood to the arteries.
- Contraction of the ventricles is coordinated by a series of specialized structures that channel the cardiac action potential through specific pathways within the ventricles: From the AV node, the cardiac action potential enters a structure called the bundle of His, then to the left and right bundle branches, and finally to the Purkinje fibers; then the ventricles contract.
The electrical impulses in the heart caused by the cardiac action potentials produce electrical currents that flow through the body and can be measured on the skin using electrodes. This information can be observed as an electrocardiogram (ECG), which is a recording of the electrical impulses of the cardiac muscle.
This video relates the cardiac cycle and cardiac action potentials to the ECG:
Regulation of Cardiac Output, Blood Pressure and Heart Rate
The information below was adapted from OpenStax Biology 40.4
Cardiac output is the volume of blood pumped by the heart in one minute. It is calculated by multiplying the heart rate (number of heart contractions that occur per minute) by the stroke volume (the volume of blood pumped into the aorta per contraction of the left ventricle).
Cardiac output can be increased by any process that increases either heart rate or stroke volume:
- Increased heart rate can occur during exercise, for example
- Increased stroke volume can occur if the heart contracts with greater strength, or if blood circulation speeds up which causes more blood to enter the heart between contractions
Regulation of cardiac output, blood pressure, and heart rate are important for ensuring sufficient blood flow to various tissues under different conditions. For example, during heavy exertion, the blood vessels in the muscles relax and increase in diameter to increase blood flow; however, this process can result in a dangerous drop in blood pressure in the body if nothing else changes. A drop in blood pressure is detected by mechanoreceptors called baroreceptors which are located in the aorta; these baroreceptors signal the brain stem, which then initiates a number of compensatory responses via the autonomic nervous system:
- cardiac output increases due to increased stroke volume and increased heart rate
- arterioles constrict the capillary beds in non-critical tissues, such as skin and intestines, diverting blood to more critical organs
- veins constrict, decreasing the overall cross-sectional area of the circulatory system

