Learning Objectives
- Identify and describe functions of key anatomical reproductive structures present in various types of animals, including the spermatheca, the cloaca, the ovary and related structures, and the testes and related structures
- Compare and contrast the process, products, and locations of male and female gametogenesis in mammals
- Describe roles of hormones in gametogenesis (spermatogenesis and oogenesis), ovulation, and implantation in placental mammals
- Explain how various medical interventions affect reproductive cycles and fertilization
Diversity of Animal Reproductive Anatomy
The information below was adapted from OpenStax Biology43.2
Many animal reproductive structures are very similar, even across different lineages. Reproductive structures produce gametes (eggs and sperm) and facilitate the meeting of gametes to produce a zygote (fertilized egg). In animals ranging from insects to humans, males produce sperm in testes, and the sperm are stored in the epididymis until ejaculation. Sperm are small, mobile, “low-cost” cells that are produced in high numbers. Females produce one ovum or several ova (eggs) that mature in the ovary. Eggs are large cells that require a substantial investment of time, energy, and nutrients to form, are non-mobile, and are rare relative to sperm numbers. Mature eggs are released from the ovary into the uterine tubes (aka fallopian tubes or oviducts) where they are either fertilized (animals that reproduce via internal fertilization), or are released in an aqueous environment (animals that reproduce via external fertilization).
The first half of Hank Green’s video below has a nice summary of these and other ideas we’ve discussed previously, and the second half introduces human reproductive anatomy before we take a deep dive into the structures and functions via dynamic hormonal regulation:
For sexually reproducing populations, we can biologically define females as the sex with ovaries that produce small numbers of large eggs, which subsequently travel down a uterine tube; and males as the sex with testes that produce large numbers of small sperm, stored in an epididymis. While this general anatomy holds true, here are some interesting differences in different animal lineages:
- Spermatheca: The spermatheca is a specialized sperm-storing sac present in females in some invertebrate species. Spermatheca are common in many insects, some mollusks, and some worms. After mating, the female stores the male’s sperm in the spermatheca for later use, sometimes up to a year or more. Fertilization can then be timed with environmental or food conditions that are optimal for offspring survival. Sperm may be stored from one male or from multiple males, depending on the species mating system. In some species, the female may mate only once in her lifetime, and use the sperm from this single mating to fertilize eggs throughout her life.
- Cloaca: The cloaca is a single, shared body opening that functions in the digestive, excretory (urine), and reproductive systems. Cloacas are found among many non-mammal vertebrates, such as most birds and reptiles. Mating between birds or reptiles usually involves positioning the cloaca openings opposite each other for transfer of sperm from male to female. Ducks are a rare exception, where the males have a penis.
- Uterus: The uterus is a structure present in placental mammals (not all mammals have a uterus!) which houses the developing offspring internal to the mother’s body. The uterus essentially serves as the location for development of an amniotic egg that is retained within the body. Depending on the species, the uterus may have two chambers in species that produce multiple offspring at a time (such as mice), or only one chamber in species that produce one offspring, (such as primates).
Mammalian (Human) Reproductive Anatomy, Gametogenesis, and Hormonal Regulation
The information below was adapted from OpenStax Biology 43.3
The remainder of this reading will focus on mammalian reproduction, featuring humans as a model organism. We’ll first look at females and then males, emphasizing the structures, the process of gametogenesis, and hormonal control of reproduction.
Gametogenesis is the production of gametes, or sperm and eggs. Gametogenesis requires meiosis (see the Biological Principles textbook page on Cell Division for help with this often confusing concept). Meiosis produces haploid cells with half the number of chromosomes normally found in diploid cells.
Hormones regulate gametogenesis in both male and female reproductive cycles, including some of the same hormones. For example, follicle stimulating hormone (FSH) and luteinizing hormone (LH) are named after their functions in egg production in females, but they play important roles in sperm production in males as well.
Human Female Reproductive Anatomy
Human female reproductive structures include both external and internal structures. External structures include the breasts and the vulva. Internal structures include ovaries, oviducts, the uterus, and the vagina, shown below.
This table briefly summarizes the major organs, locations, and functions of mammalian female reproductive anatomy:
| Organ | Function |
|---|---|
| Ovaries | Produces and develops (matures) eggs |
| Fallopian tubes (oviducts) | Site of fertilization; transports egg to uterus |
| Uterus | Supports developing embryo |
| Cervix | Allows passage between the uterus and the vagina |
| Vagina | Receives penis during intercourse, acts as birth canal, passes menstrual flow |
| Breasts | Produce and deliver milk |
Human females become capable of reproduction at sexual maturity, which follows puberty. During puberty, the hypothalamus in the brain signals the pituitary gland to produce two hormones, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In females, FSH and LH stimulate the ovaries to produce the female sex hormones, estrogen and progesterone. During puberty, these hormones initiate development of secondary sex characteristics (such as breasts) and cause the ovaries to begin producing mature eggs.
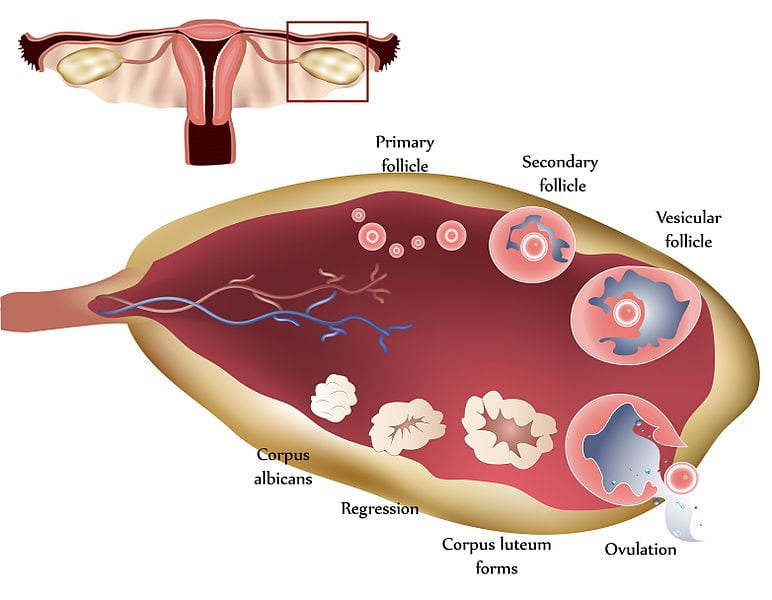
Ovaries are the site of egg development and maturation. Eggs develop and mature in structures called follicles, which are found throughout the ovary. Each follicle contains one immature egg. Egg development in humans occurs in small batches, with one or two eggs maturing on an approximately-monthly cycle called the ovarian cycle:
- In the first phase of the ovarian cycle, the several follicles become activated to promote development of the egg inside of them (recall that each follicle contains one immature egg).
- At the middle of the ovarian cycle, the most mature follicle will “rupture,” releasing one egg as illustrated below (rarely, a second follicle will rupture, resulting in ovulation of two eggs). The egg travels from the ruptured follicle into the oviducts (also called fallopian tubes), where it will be fertilized if sperm are present. Over the course of about a week, the egg will travel through the oviduct into the uterus, where it will implant and result in pregnancy if fertilization previously occurred in the oviduct. Fertilization must take place in the oviduct, not the uterus.
- In the last phase of the ovarian cycle, the ruptured follicle (still in the ovary) becomes the corpus luteum, which secretes hormones that prevent menstruation until the egg has had time to be fertilized. If fertilization and implantation in the uterine wall occurs, then the corpus luteum continues to prevent menstruation; if fertilization does not occur, then the corpus luteum degenerates and menstruation occurs.
Female Gametogenesis: Oogenesis
Now that we have discussed the human female reproductive structures, let’s walk through the process of oogenesis, or egg production.
The process of oogenesis begins while the female herself is still an embryo! Oogenesis occurs in the ovaries, where egg stem cells, called oogonia, divide by mitosis to produce up to 2 million oocytes (a precursor to the egg). The oocytes start the process of meiosis, and then pause during meiosis I. This process occurs during embryonic development, meaning that a female mammal is born with every single egg she will be able produce during her lifetime already present (in an immature form) in her ovaries. This situation is very different from males, whose spermatogonia (the sperm equivalent to oogonia) do not begin producing spermatocytes (the sperm equivalent to oocytes) until puberty.
The oocytes remain paused in meiosis I until the onset of puberty, when a series of events can lead to egg maturation on an approximately monthly basis:
- Hormones from the pituitary cause some of the follicles to begin developing and the oocyte inside the follicle to finish meiosis I (recall that each follicle contains one immature egg).
- After completing meiosis I, the oocyte pauses during meiosis II.
- Though several follicles are activated during each cycle, typically only one follicle will release an oocyte. The released oocyte will begin traveling through the oviduct, still paused in meiosis II.
- If the oocyte is fertilized by a sperm cell, it will finish meiosis II to produce a single fertilized egg (a zygote). If it is not fertilized, the oocyte degrades without completing meiosis II.
One final point: when each oocyte undergoes meiosis to go from diploid to haploid, each oocyte produces only a single egg (this is different from spermatogenesis, which produces four sperm from each spermatocyte). The oocyte undergoes a process called unequal cytokinesis, meaning it divides unequally so that almost all of the cytoplasm goes into only one daughter cell rather than evenly distributed into both. The smaller cell is called a polar body, and it normally dies as development progresses.
The process of oogenesis is illustrated below:

Hormonal Control of Oogenesis
Now that we have discussed the structures and the processes of oogenesis, we’ll move into the most complex part: hormonal regulation of oogenesis. Oogenesis is directly controlled by four hormones: follicle stimulating hormone (FSH), luteinizing hormone (LH), progesterone, and estrogen. These hormones together regulate the ovarian and menstrual cycles. The ovarian cycle refers to the release of eggs, and the menstrual cycle refers to activities in the uterine lining in preparation for possible pregnancy. We will focus only on the ovarian cycle in this course.
We’ll start with a brief overview of the roles the hormones play:
- Follicle stimulating hormone (FSH) activates follicles within the ovary to promote development of egg cells, causing eggs to finish meiosis I and pause during meiosis II. (Recall that each follicle contains one immature egg cell which was paused in meiosis I.)
- Luteinizing Hormone (LH) promotes release of the most mature egg (or in rare cases, eggs), resulting in ovulation
- Progesterone suppresses release of more FSH or LH to block activation of new follicles, allowing time for the ovulated egg to be fertilized in the oviduct and then travel to the uterus where it will implant if previously fertilized.
- Estrogen can be thought of as an ‘enhancer’ in the ovarian cycle; it enhances the activation of follicles in response to FSH, and it also enhances suppression of follicles in response to progesterone. (Estrogen also has other roles outside of the ovarian cycle, including re-growing the lining of the uterus following menstruation, and it is responsible for the secondary sexual characteristics of females such as breast development.)
Now we’ll integrate the hormone activities into the three phases of the ovarian cycle. The ovarian cycle lasts approximately 28 days on average:
Follicular phase: The first half of the ovarian cycle is the follicular phase, named for the fact that the dominant feature is the activated follicles.
- During this phase, FSH is being released from the pituitary in the brain. The slowly rising levels of FSH prompt the follicles on the surface of the ovary to grow and begin maturing the egg inside for ovulation.
- As the follicles grow, they release estrogens. Estrogens enhance the effects of FSH. The more the follicles grow, the more estrogen they release; the increasing estrogen levels cause a positive feedback loop promoting more follicle growth, which in turn promotes more estrogen release.
- Within each follicle, the maturing egg finishes meiosis I (recall that the eggs began meiosis I while the female herself was an embryo), and then pauses again during meiosis II.
Ovulation occurs near the middle of the cycle (approximately day 14), when the high level of estrogen (produced by the developing follicles) causes a rapid rise and sharp spike in levels of LH and FSH to a lesser degree (both released from the pituitary in the brain).
- The spike in LH causes ovulation: one of the mature follicles ruptures and releases its egg (still paused in meiosis II). The other mature follicles will degenerate, and their eggs are lost.
- LH and FSH levels fall immediately after ovulation, and the level of estrogen decreases when the extra follicles degenerate.
- It takes about seven days for an egg to travel through the oviduct from the ovary to the uterus, and it must be fertilized while in the oviduct. If the egg is fertilized, it will complete meiosis II, producing a single mature (and fertilized) egg.
Luteal phase: Following ovulation, the ovarian cycle enters its luteal phase, named for the fact that the dominant feature is the corpus luteum, the structure the remains from the ruptured follicle.
- During this phase, the corpus luteum produces progesterone and estrogen. Progesterone inhibits the release of further FSH or LH, suppressing activation of any new follicles. The uterus becomes prepared to accept a fertilized egg, should fertilization occur.
- The inhibition of FSH and LH by progesterone prevents any further eggs and follicles from developing. The level of estrogen produced by the corpus luteum increases to a steady level for the next few days; estrogen enhances the effects of progesterone.
What happens next depends on whether the egg was fertilized while it was in the oviduct:
- If a fertilized egg does not implant into the endometrial lining of the uterine wall, then the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The decrease in progesterone releases the suppression on FSH; the anterior pituitary then releases FSH which starts the cycle again.
- If a fertilized egg does implant in the endometrial lining of the uterine wall, then embryo produces a hormone called human chorionic gonadotropin (hCG). hCG causes the corpus luteum to remain instead of degrading, which in turn causes the ovary to continue producing high levels of progesterone. Progesterone prevents initiation of another ovarian cycle during the pregnancy. (The placenta takes over this process later in pregnancy.) Because hCG is unique to pregnancy, it is the hormone detected by pregnancy tests.
The figure below visually compares the ovarian and uterine cycles as well as the hormone levels controlling these cycles.

This video provides a great overview of the human female reproductive system, emphasizing many of the points described above:
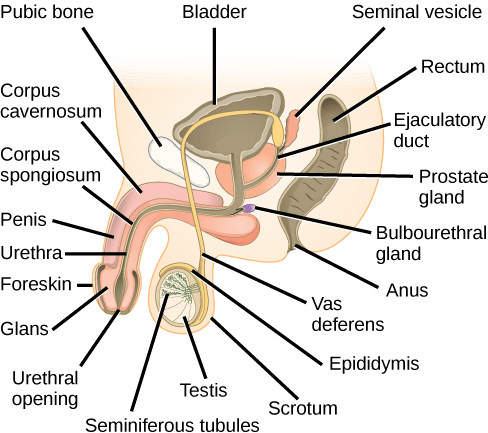
Human Male Reproductive Anatomy
As with females, human male reproductive structures include both external and internal structures. External structures include the testicles or testes (singular: testis) and the penis. Internal structures include the vas deferens, the seminal vesicles, the prostate gland, and the bulbourethral gland.
This table briefly summarizes the major organs, locations, and functions of mammalian male reproductive anatomy:
| Organ | Location | Function |
| Scrotum | External | Carry and support testes |
| Penis | External | Deliver urine, copulating organ |
| Testes | External | Produce sperm and male hormones |
| Seminal vesicles | Internal | Contribute to semen production |
| Prostate gland | Internal | Contribute to semen production |
| Bulbourethral glands | Internal | Clean urethra at ejaculation |
Human males become capable of reproduction at sexual maturity, which follows puberty. During puberty, the hypothalamus in the brain signals the pituitary gland to produce two hormones, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In males, FSH and LH stimulate the testes to produce sperm and the male sex hormone, testosterone. During puberty, these hormones together initiate development of secondary sex characteristics (such as larger penis and testes, and deeper voice) and cause the testes to begin producing mature sperm.
The scrotum houses the testes or testicles (singular: testis), which are the site of sperm development and maturation. Testes develop from the same tissue that produces ovaries in females; however, in terrestrial mammals, the cells that produce the testes migrate from within the body cavity to become external to the body during development. Why are testes external to the body in terrestrial mammals? Sperm become immobile when kept at body temperature; therefore, the scrotum and penis are external to the body in land mammals and kept at about 2° C lower than body temperature to maintain sperm motility. In cases where the testes do not descend through the abdominal cavity during fetal development, infertility can occur in land mammals due to the higher body temperature. Though sperm must be produced and stored at temperatures lower than body temperature in the testes, sperm are warmed to body temperature when deposited in the female reproductive tract. The immediate warming of sperm causes them to experience a burst of swimming activity, but then they begin to lose motility after several hours at body temperature.
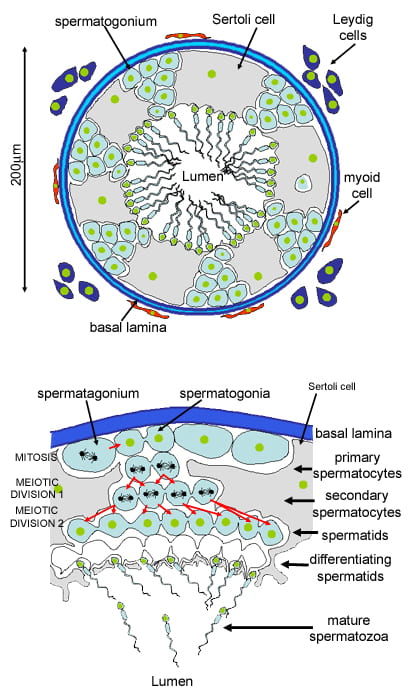
Within the testes, sperm are produced in structures called the seminiferous tubules. Sperm production is regulated by Sertoli cells which protect the sperm stem cells and promote their development, and cells of Leydig which produce testosterone and regulate sperm development. Sperm mature as they proceed from the periphery to the lumen (interior) of the seminiferous tubules.
When the sperm have developed flagella and are nearly mature, they leave the testes and enter the epididymis, a structure which wraps around the testes and the location where sperm mature. During ejaculation, the sperm leave the epididymis and enter the vas deferens, which carries the sperm, behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles.
Semen is a mixture of sperm and spermatic duct secretions and fluids from accessory glands. These glands are the seminal vesicles, the prostate gland, and the bulbourethral gland (all of which are illustrated above); together these glands contribute most of the semen’s volume:
- The seminal vesicles are a pair of glands that make thick, yellowish, and alkaline solution. Because sperm are only motile in an alkaline environment, a basic pH is important to reverse the acidity of the vaginal environment. The solution also contains mucus, fructose (a source of energy for the sperm cells), a coagulating enzyme, ascorbic acid (vitamin C), and local-acting hormones called prostaglandins (may help stimulate smooth muscle contractions in the uterus). The seminal vesicle glands account for 60 percent of the bulk of semen.
- The prostate gland acts as both a muscle and a gland. The muscle provides much of the force for ejaculation to occur. The glandular tissue makes a thin, milky fluid that contains citrate (stimulates sperm motility), enzymes, and prostate specific antigen (PSA). PSA is a proteolytic enzyme that helps to liquefy the ejaculate several minutes after release from the male. Prostate gland secretions account for about 30 percent of the bulk of semen.
- The bulbourethral gland releases its secretion just before the release of the bulk of the semen. The mucous secretions of this gland help lubricate and neutralize any acid residue in the urethra left over from urine. Secretions from the bulbourethral gland can also contain a few sperm; since these secretions are released prior to ejaculation, withdrawal of the penis from the vagina before ejaculation to prevent pregnancy may not work if sperm are present in the bulbourethral gland secretions.
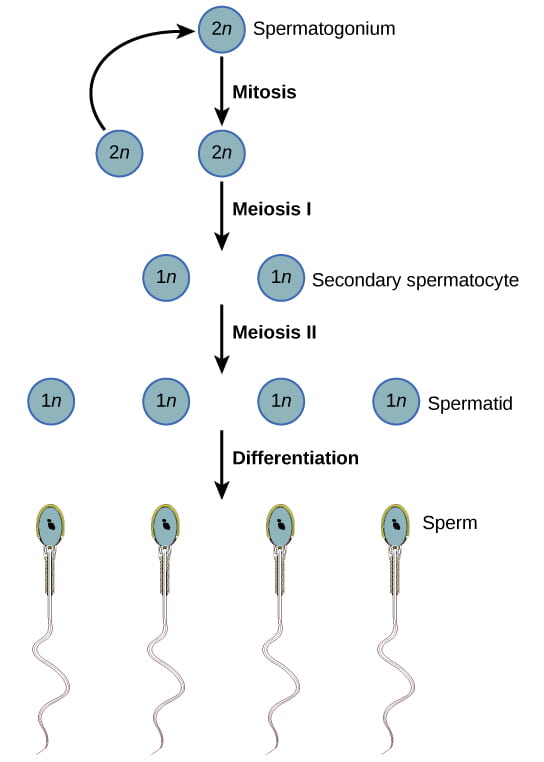
Male Gametogenesis: Spermatogenesis
Spermatogenesis, illustrated below, occurs in the seminiferous tubules in the testes. Sperm stem cells, called spermatogonia, are present at birth but are inactive until puberty, when hormones from the pituitary cause the activation of the spermatogonia and the continuous production of sperm. Sperm production continues into old age. To produce sperm, a cell called a spermatocyte (a precursor to sperm) undergoes meiosis to produce four haploid spermatids (immature sperm). Once the spermatid develops a flagellum, (a tail that allows it to swim), it is called a sperm cell. Four sperm cells result from each spermatocyte that goes through meiosis. (Scroll up to compare this process to oogenesis in human females, and see how many similarities and differences you can identify.)
Hormonal Control of Spermatogenesis
The information below was adapted from OpenStax Biology 43.4
Now that we have discussed the structures and processes of spermatogenesis, we’ll move into discussion of hormone regulation. Just like oogenesis, spermatogenesis is controlled by follicle-stimulated hormone (FSH) and luteinizing hormone (LH). Testosterone also plays a role in spermatogenesis:
- FSH stimulates activity of the Sertoli cells to nourish the developing sperm and promote their development. Sertoli cells are located within the seminiferous tubules, and play an analogous role to follicle cells in the ovaries.
- LH stimulates the Leydig cells to produce testosterone, which promotes spermatogenesis. Leydig cells are located in the testes, outside of the seminiferous tubules.
- Testosterone further stimulates spermatogenesis by promoting maturation of the sperm after completing meiosis.
While this doesn’t occur in a monthly cycle as in females, the hormones do interact in a negative feedback cycle when sperm counts get too high (over about 20 million/ml): rising testosterone levels cause Sertoli cells to release the hormone inhibin, which acts on the hypothalamus and pituitary gland to inhibit the release of FSH and LH. The inhibition causes spermatogenesis to slow down; once the sperm levels are reduced, the Sertoli cells stop releasing inhibin, and the sperm count increases.
This video provides a great overview of the anatomy and function of the human male reproductive system:
Oogenesis vs Spermatogenesis
As we’ve seen in this reading and the videos, both eggs and sperm are produced via meiosis, but there are some big differences:
- Initiation: Egg production begins during embryonic development (before birth), then is arrested during meiosis until puberty; sperm production does not begin until puberty
- Completion: Egg production is not actually completed until after fertilization (!), while sperm production is complete prior to ejaculation
- Number: Egg production results in only a single egg from each egg stem cell; sperm production results in four sperm from each sperm stem cell.
- Timing: Once an individual enters puberty, sperm production is continuous in a “conveyor belt” process; egg production occurs one-at-a-time at each menstrual cycle.
Contraception and Birth Control
The information below was adapted from OpenStax Biology 43.5
We’ll wrap this discussion up with an overview of contraception. Contraception (prevention of pregnancy), can be categorized by according to whether they block gamete production or gamete union (fertilization):
- Blocking gamete production: hormone-based birth control methods block gamete production, and so far they are only available for female gamete production (though there has long been interest and research in identifying a method to inhibit sperm production in males).
- Hormone-based birth control methods use synthetic progesterone (sometimes in combination with estrogen), which inhibits production of FSH and LH, and thus prevent an egg from being maturing or being released. Progesterone is the primary hormone that blocks FSH and LH release, but estrogen enhances its effect and increases the reliability of this method. This method includes “the pill” as well as other methods of delivering the hormone(s) such as implants under the skin; methods such as skin implants are more reliable due to the continuous release of progesterone.
- Intrauterine devices (IUDs) are small T-shaped devices that are inserted into the uterus. IUDs induce an inflammatory response in the uterus that creates a toxic environment to the sperm and prevents them from reaching the oviducts. Some IUDs that contain progesterone which is continually secreted to suppress egg production and ovulation; others are copper-coated which alters the cervical mucus making it more difficult for sperm to reach the egg. Both types of IUDs are more reliable than standard hormone-based birth control.
- Emergency contraception, also known as “Plan B” or the “morning-after pill” is a hormone-based method of contraception containing a high dose of synthetic progesterone, which temporarily blocks egg maturation and ovulation, allowing time for sperm to die in the oviduct before the egg is released. It can also act after ovulation slowing down movement of the egg and thickening cervical mucus which slows movement of sperm. One common misconception about emergency contraception is that it prevents implantation after fertilization; however, it has no impact after fertilization.
- Blocking gamete union (fertilization): methods to block union between sperm and egg include barrier methods such as condoms, spermicides, vasectomy, and tubal ligation.
- Barrier methods, such as condoms, cervical caps, and diaphragms, block sperm from entering the uterus, preventing fertilization. Spermicides are chemicals that are placed in the vagina that kill sperm. Sponges, which are saturated with spermicides, are placed in the vagina at the cervical opening. Combining spermicides with barrier methods is more effective than using either alone.
- Vasectomies block sperm from exiting the body during ejaculation (contrary to popular misconception, vasectomies do not block sperm production – only sperm release). A section of the vas deferens is removed, so sperm are still produced but cannot reach the urethra to be ejaculated. No other structures are affected, and so all other components of ejaculate are still present. Vasectomy is one of the most effective methods of birth control.
- Tubal ligation is the female equivalent to a vasectomy in that it involves severing and sealing the oviducts; eggs are still produced and ovulated from the ovaries, but they are unable to reach the oviducts for fertilization. However, unlike vasectomies which are performed through the scrotum, tubal ligation requires abdominal surgery to reach the oviducts. Tubal ligation is also among the most effective methods of birth control.
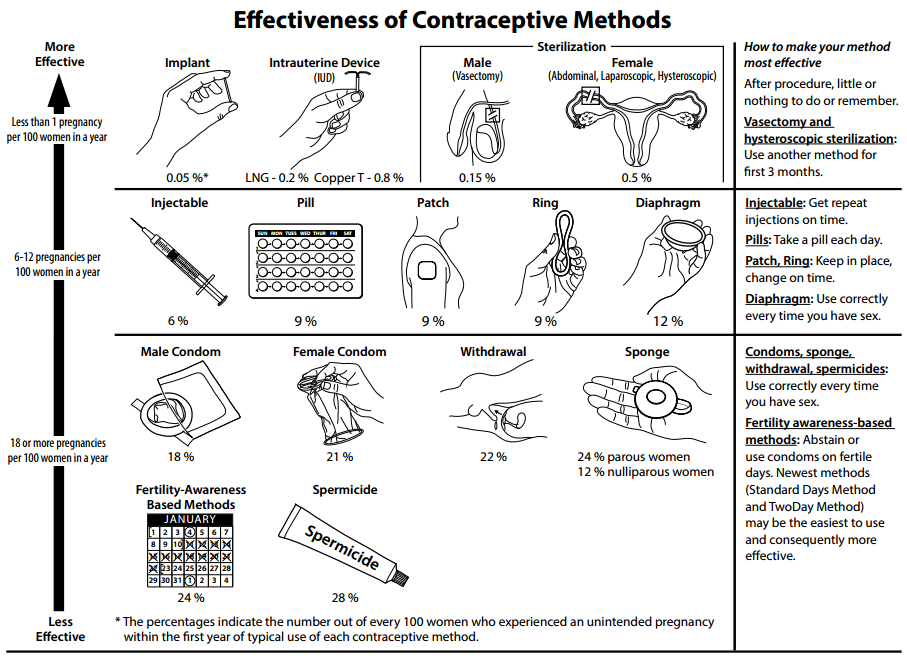
Methods of contraception to prevent pregnancy have varying probabilities of success. In the diagram below, the failure rate is the given as the percent of women who become pregnant during the first year of use of that method. Work through the methods in this diagram to determine the most effective strategies for preventing pregnancy. Methods in combination, such as spermicidal chemicals and barrier, prevent pregnancy more effectively than do the methods when used separately.
This video provides a quick overview of hormone-based birth control, with emphasis on emergency contraception: