Learning Objectives
- Describe the structure and function of the mammalian kidney
- Describe the structure and function of each region of the mammalian nephron, including the glomerulus, Bowman’s capsule, proximal convoluted tubule, Loop of Henle, distal convoluted tubule, collecting duct, and associated capillary network including the vasa recta
- Describe the blood filtration process of the nephron, and recognize the roles of active and passive transport, osmotic gradients, and countercurrent exchange in nephron function
- Explain the roles of aldosterone and antidiuretic hormone in osmoregulation by the mammalian kidney
The Mammalian Kidney
The information below was adapted from OpenStax Biology 41.2
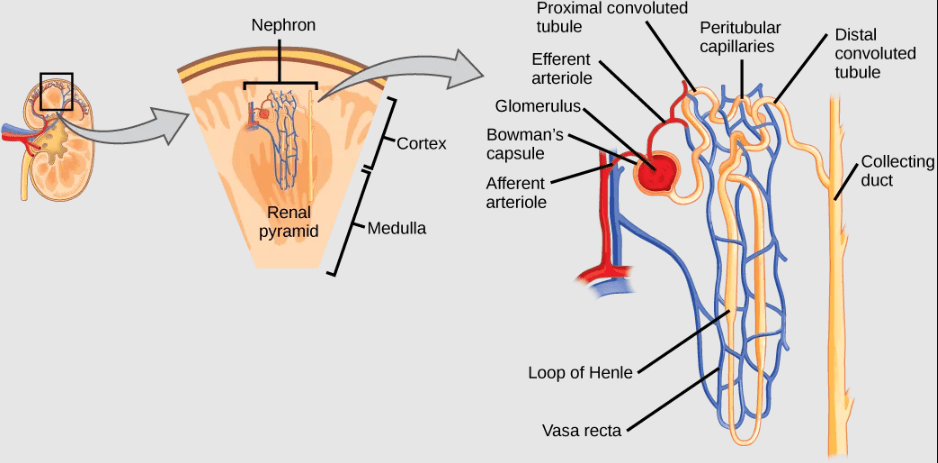
The kidneys, a pair of bean-shaped organs located just below and behind the liver, are the major osmoregulatory organ in mammals. Kidneys filter blood and purify it, producing a filtrate called urine. The functional unit of the kidney is called the nephron. Each kidney has three internal regions: an outer cortex, a medulla in the middle, and the renal pelvis in the region called the hilum of the kidney.
- The renal cortex, or outer layer of the kidney interior, contains the nephrons, which perform filtration and osmoregulation by the kidneys.
- The medulla, the middle layer of the kidney interior, consists of multiple pyramidal tissue masses, called the renal pyramids. In between the pyramids are spaces called renal columns through which the blood vessels pass. The tips of the pyramids, called renal papillae, point toward the renal pelvis. The medulla has a higher concentration of salt compared to the cortex.
- On the inside of the kidney, the renal pelvis contains the arteries, veins, and nerves that supply the kidney. The ureters are urine-bearing tubes that exit the kidney and empty into the urinary bladder.
Structure of the Mammalian Nephron
The information below was adapted from OpenStax Biology 41.2
As mentioned previously, the functional unit of the kidney is the nephron. Each kidney is made up of over one million nephrons that dot the renal cortex, giving it a granular appearance. There are two types of nephrons: cortical nephrons (85 percent), which are deep in the renal cortex, and juxtamedullary nephrons (15 percent), which lie in the renal cortex close to the renal medulla. Though juxtamedullary nephrons are far less common than cortical nephrons, they play a critical role in helping to set up the salt concentration gradient of the medulla, which facilitates reabsorption of water from the pre-urine filtrate.
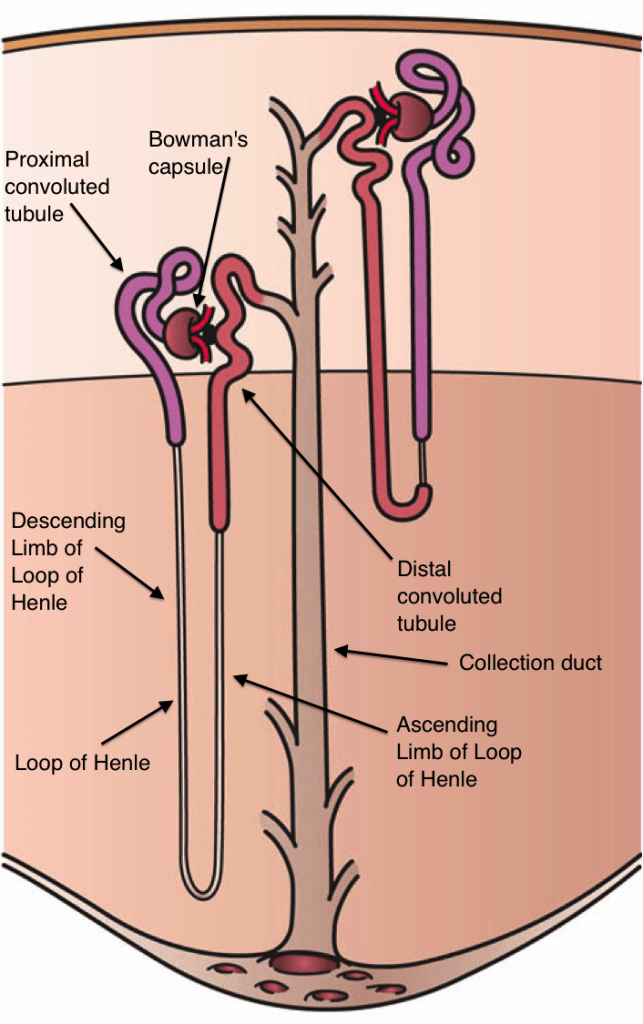
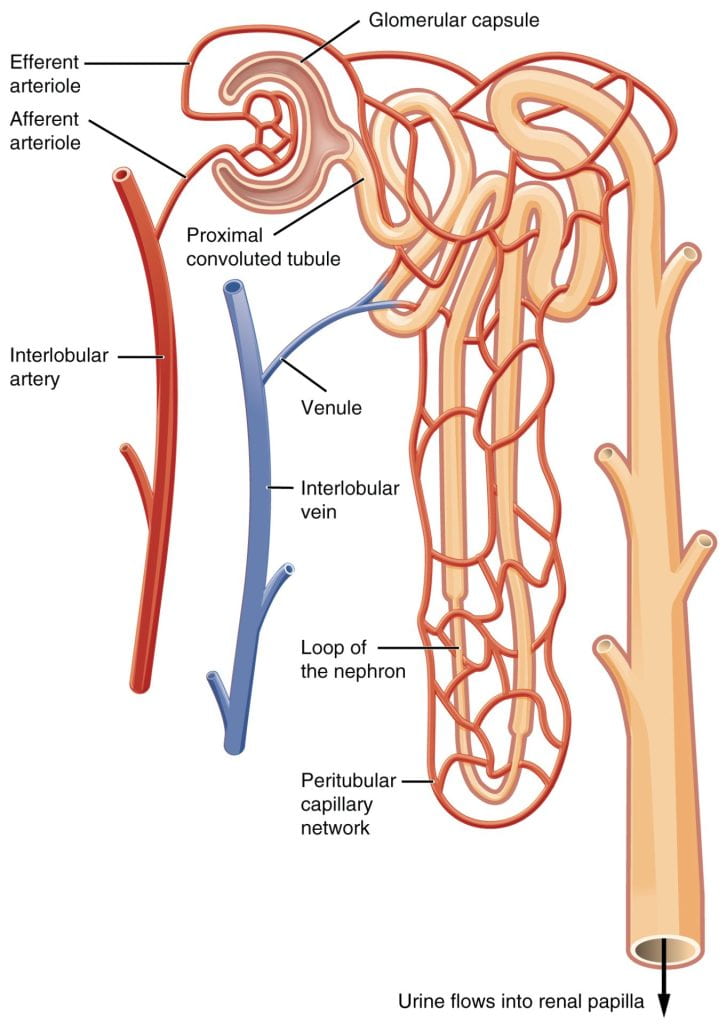
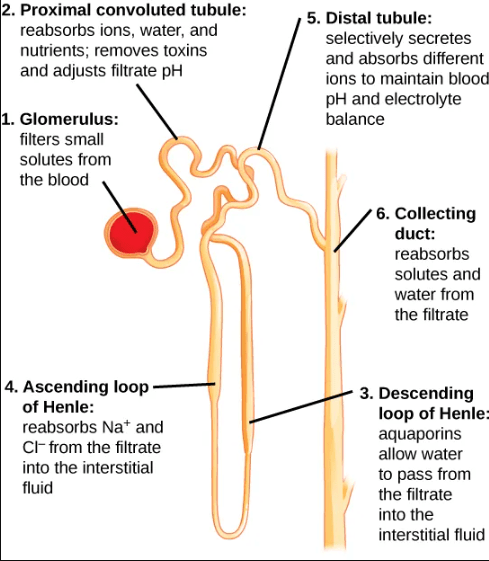
A nephron consists of three parts: a renal corpuscle, a renal tubule consisting of three parts (the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule), and the associated capillary network, which originates from the cortical radiate arteries and includes the vasa recta which surrounds the loop of Henle. Each nephron empties into a shared collecting duct which transports urine to the bladder.
- The renal corpuscle, located in the renal cortex, is made up of a network of capillaries known as the glomerulus and the capsule, a cup-shaped chamber that surrounds it, called the glomerular or Bowman’s capsule.
- The renal tubule is a long and convoluted structure that emerges from the glomerulus and can be divided into three parts based on function:
- The first part is called the proximal convoluted tubule due to its proximity to the glomerulus; it stays in the renal cortex.
- The second part is called the loop of Henle, or nephritic loop, because it forms a loop (with descending and ascending limbs) that goes through the renal medulla.
- The third part of the renal tubule is called the distal convoluted tubule, and this part is also restricted to the renal cortex. The DCT, which is the last part of the nephron, connects and empties its contents into collecting ducts that line the medullary pyramids.
- The collecting ducts amass contents from multiple nephrons and fuse together as they enter the papillae of the renal medulla.
- The capillary network that originates from the renal arteries supplies the nephron with blood that needs to be filtered. The branch that enters the glomerulus is called the afferent arteriole. The branch that exits the glomerulus is called the efferent arteriole. Within the glomerulus, the network of capillaries is called the glomerular capillary bed. Once the efferent arteriole exits the glomerulus, it forms the peritubular capillary network, which surrounds and interacts with parts of the renal tubule. In cortical nephrons, the peritubular capillary network surrounds the proximal convoluted tubule and distal convoluted tubule. In juxtamedullary nephrons, the peritubular capillary network forms a network around the loop of Henle and is called the vasa recta.
Blood Filtration by the Nephron
Kidneys filter blood in a multi-step process:
- First, the nephrons filter blood that runs through the capillary network in the glomerulus. Almost all solutes, except for proteins, are filtered out into the glomerulus by a process called glomerular filtration.
- Glomerular filtration filters out most of the solutes due to high blood pressure and specialized membranes in the afferent arteriole. The blood pressure in the glomerulus is maintained independent of factors that affect systemic blood pressure. The “leaky” connections between the endothelial cells of the glomerular capillary network allow solutes to pass through easily. All solutes in the glomerular capillaries, except for macromolecules like proteins, pass through by passive diffusion.
- Filtration by the glomerulus is nonspecific, and there is no energy requirement at this stage of the filtration process.
- Second, the filtrate is collected in the renal tubules. Most of the solutes get reabsorbed in the proximal collecting tubule by a process called tubular reabsorption. In the loop of Henle, the filtrate continues to exchange solutes and water with the renal medulla and the peritubular capillary network. Water is also reabsorbed during this step.
- Tubular reabsorption occurs in the proximal convoluted tubule part of the renal tubule. Almost all nutrients are reabsorbed, and this occurs either by passive or active transport. Reabsorption of water and some key electrolytes are regulated and can be influenced by hormones. Sodium (Na+) is the most abundant ion and most of it is reabsorbed by active transport and then transported to the peritubular capillaries. Because Na+ is actively transported out of the tubule, water follows it to even out the osmotic pressure. Water is also independently reabsorbed into the peritubular capillaries due to the presence of aquaporins, or water channels, in the proximal convoluted tubule. This phenomenon occurs due to the low blood pressure and high osmotic pressure in the peritubular capillaries.
- Reabsorption of nutrients, vitamins, and ions in the proximal convoluted tubule is an active process, requiring ATP; water follows passively by osmosis.
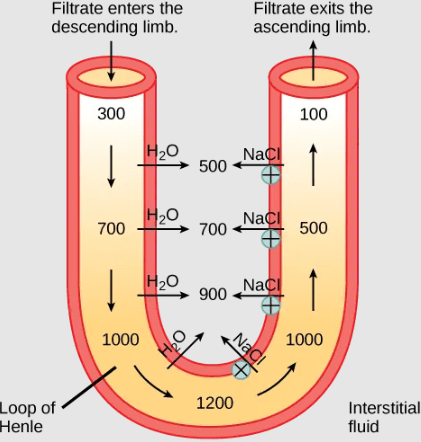
- In the loop of Henle, the permeability of the membrane changes. The descending limb is permeable to water, not solutes; the opposite is true for the ascending limb. Additionally, the loop of Henle invades the renal medulla, which is naturally high in salt concentration and tends to absorb water from the renal tubule and concentrate the filtrate. The osmotic gradient increases as it moves deeper into the medulla. Because two sides of the loop of Henle perform opposing functions, it acts as a countercurrent multiplier. The vasa recta around it acts as the countercurrent exchanger.
- The loop of Henle utilizes countercurrent flow, selective permeability that changes across the loop, as well as both active and passive transport of ions; water follows passively by osmosis.
- By the time the filtrate reaches the distal convoluted tubule, most of the urine and solutes have been reabsorbed. If the body requires additional water, water can be reabsorbed at this point. Further reabsorption is controlled by hormones, discussed below. Excretion of wastes occurs due to lack of reabsorption combined with tubular secretion. Undesirable products like metabolic wastes, urea, uric acid, and certain drugs, are excreted by tubular secretion. Most of the tubular secretion happens in the distal convoluted tubule, but some occurs in the early part of the collecting duct. Kidneys also maintain an acid-base balance by secreting excess H+ ions. Additional solutes and wastes are secreted into the kidney tubules during tubular secretion, which is, in essence, the opposite process to tubular reabsorption.
- Reabsorption of water, ions, and urea in the distal convoluted tubule includes passive and active transport, and this reabsorption is regulated by hormones.
- Tubular reabsorption occurs in the proximal convoluted tubule part of the renal tubule. Almost all nutrients are reabsorbed, and this occurs either by passive or active transport. Reabsorption of water and some key electrolytes are regulated and can be influenced by hormones. Sodium (Na+) is the most abundant ion and most of it is reabsorbed by active transport and then transported to the peritubular capillaries. Because Na+ is actively transported out of the tubule, water follows it to even out the osmotic pressure. Water is also independently reabsorbed into the peritubular capillaries due to the presence of aquaporins, or water channels, in the proximal convoluted tubule. This phenomenon occurs due to the low blood pressure and high osmotic pressure in the peritubular capillaries.
- The collecting ducts collect filtrate coming from the nephrons and ultimately deliver the filtrate, now called urine, to the ureters and finally the bladder.
- Reabsorption of water by the collecting ducts is a passive and hormone-regulated process.
This video provides an overview of the mammalian excretory system:
And this video provides a step-by-step description of mammalian kidney function: http://www.sumanasinc.com/webcontent/animations/content/kidney.html
Hormonal Regulation of Osmoregulation in Mammals
The information below was adapted from OpenStax Biology 41.5
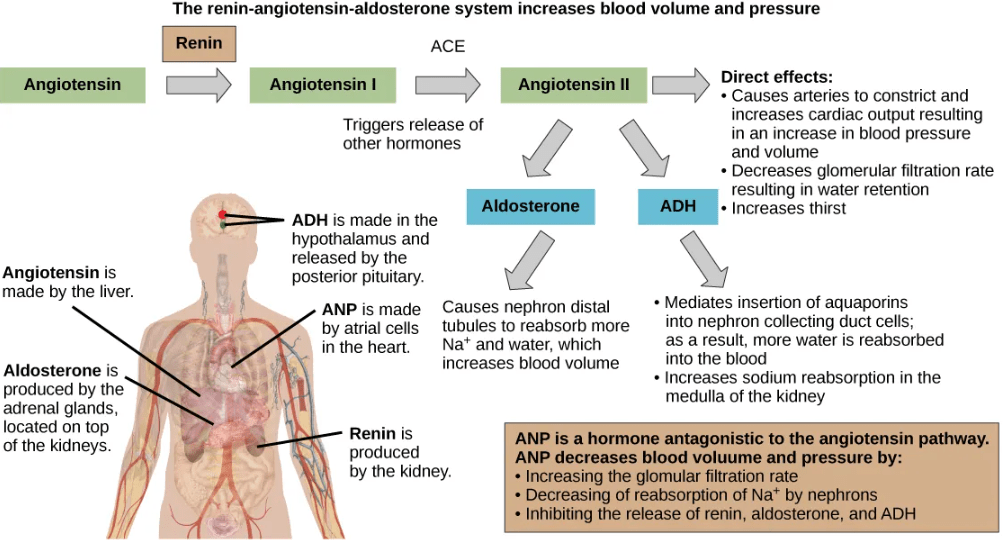
While the kidneys operate to maintain osmotic balance and blood pressure in the body, they also act in concert with hormones. As a reminder, hormones are small molecules that act as messengers within the body. Hormones are typically secreted from one cell and travel in the bloodstream to affect a target cell in another portion of the body. Different regions of the nephron bear specialized cells that have receptors to respond to chemical messengers and hormones. Though there are multiple hormones which regulate mammalian nephron function, here we will focus on just two: aldosterone and antidiuretic hormone.
- Aldosterone is a mineralocorticoid synthesized by the adrenal cortex that regulates sodium levels in the blood. Almost all of the sodium in the blood is reclaimed by the renal tubules under the influence of aldosterone. Because sodium is always reabsorbed by active transport and water follows sodium to maintain osmotic balance, aldosterone manages not only sodium levels but also the water levels in body fluids. Aldosterone also stimulates potassium secretion concurrently with sodium reabsorption. The absence of aldosterone means that no sodium gets reabsorbed in the renal tubules and all of it gets excreted in the urine. In addition, the daily dietary potassium load is not secreted and the retention of K+ can cause a dangerous increase in plasma K+ concentration.
- Antidiuretic hormone or ADH (also called vasopressin) helps the body conserve water when body fluid volume, especially that of blood, is low. It is formed by the hypothalamus and is stored and released from the posterior pituitary. It acts by inserting aquaporins in the collecting ducts and promotes reabsorption of water. ADH also acts as a vasoconstrictor and increases blood pressure during hemorrhaging.
| Hormones That Affect Osmoregulation | ||
|---|---|---|
| Hormone | Where produced | Function |
| Aldosterone | Adrenal cortex | Prevents loss of sodium and water |
| Anti-diuretic hormone (vasopressin) | Hypothalamus (stored in the posterior pituitary) | Prevents water loss |